When people think of Post Traumatic Stress Disorder (PTSD), they typically visualize the “usual” ways of addressing mental health struggles, such as treatments like talk therapy, medication, and support groups. While these are indeed helpful components of healing, they are not the complete picture of what your body needs for a full recovery. In fact, you may be surprised to learn that a key element to recovery from emotional trauma is restoring the balance of bacteria in your intestines. That is correct: your gut health directly affects your mood!
If you are working through trauma recovery or know someone who is, this article is a must-read. When the gut-brain component of trauma therapy is overlooked, it may slow down or counteract efforts to overcome PTSD and other debilitating forms of mental illness, such as anxiety or depression.
In addition to trauma recovery, maintaining a balanced gut microbiome is beneficial for anyone interested in holistic methods of maintaining mental wellness. In this article, I will explain how your gut, nervous system, and brain are interconnected. You will also find several tips and resources for improving your own gut health, whether you are struggling with PTSD or simply looking to reap the benefits of a healthy gut microbiome.
UNDERSTANDING THE BRAIN-GUT AXIS:
WHY GUT HEALTH MATTERS IN PTSD RECOVERY
It may seem surprising to think about the intestines in relation to brain health, but it is imperative that healthcare providers address this link in order to provide the most comprehensive treatment plan. First, let us simplify the relationship between the brain, the gut, and the nervous system.
What does “gut health” mean, exactly?
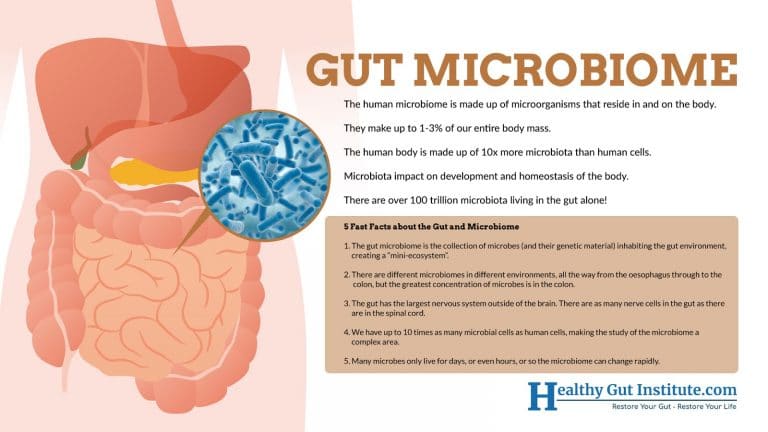
The human microbiome is made up of microorganisms that reside on and inside the body. Your intestines, or “gut” host the majority of these microorganisms and bacteria. In fact, there are more than 100 trillion gut microbiota living in your gut alone! The various strains of bacteria in your gut as a whole are referred to as gut microbiota, gut microbiome, or gut flora. It is important to have a healthy balance of “good bacteria” (probiotics) vs “bad bacteria,” and it is equally as important to have a wide diversity of strains of bacteria.
Most of your immune system is located in your gut, and the implications of this are far-reaching: a healthy gut microbiome promotes healthier skin, smoother digestion, more energy, higher resilience to ailments like the common cold, and many more health benefits. In order to understand natural ways to improve the gut microflora, I suggest checking out How Prebiotics and Probiotics Can Transform Your Health.
What does the gut have to do with the nervous system?
It is important to realize that the gut has the largest nervous system outside of the brain, and it houses many receptors responsible for stabilizing mood. These include chemicals like serotonin, dopamine, glutamate, and γ‐aminobutyric acid (GABA). An imbalanced gut can disrupt neurotransmitters and neurosteroids to the point where a person feels out of control of their feelings, has difficulty maintaining healthy relationships, or suffers a general feeling of burnout at work or school. Since these struggles are already common symptoms in individuals who suffer from PTSD, you can see how an unhealthy gut may maximize these symptoms and make recovery more difficult.
What is the “gut-brain axis”?
The gut-brain axis refers to scientific research revealing an ongoing communication between the gut microbiome, the nervous system, and the brain. Studies have shown that an unhealthy gut microbiome plays a role in the development of various psychiatric disorders. Furthermore, the bacteria in your gut sends messages to your brain through the vagus nerve, which is part of the parasympathetic nervous system. In addition to other physical processes, the signals from the vagus nerve greatly affect the cognitive and emotional functioning in the brain. As you may expect, a damaged gut sends distressing signals, activating parts of the brain responsible for anxiety, stress, memory, cognitive reasoning, and depression.
WHY THE GUT IS PARTICULARLY VULNERABLE DURING EARLY CHILDHOOD
Your body programs the way the gut and brain interact very early on in life, even during the prenatal period! Specifically, your brain-gut axis establishes its patterns during the first three years of life. That is why, if trauma occurs during early childhood, the gut is more likely to be damaged and require special attention in treatment.
The trauma-induced reshaping of the gut microbiome during early childhood creates far-reaching problems that can lead to an increased risk of psychiatric distress as an adult, as well as more physical problems.
This is because trauma causes long-lasting damage to the microbiome. Serious damage is most prevalent in severe, ongoing trauma that occurred during early childhood. In fact, this type of damage in the gut continues to send signals to the brain long after the traumatic event, evoking intense feelings of anxiety, depression, and panic. As you can see, even when a person is working hard to restore their mental health, an unhealthy gut is likely to undermine some of their efforts.

STUDIES SUGGESTING THAT BACTERIA MAY IMPACT OUTCOME AFTER TRAUMATIC EVENT
Although many people experience traumatic events during their lifetime, not everyone develops PTSD. This is because their gut health at the time of their exposure to a traumatic event may play a role in their resilience against PTSD.
For example, an exploratory study conducted by Dr. Stefanie Malan-Müller, a postdoctoral fellow in psychiatry at Stellenbosch University, examined the gut flora of individuals diagnosed with PTSD and compared them with the gut microbes of people who, while they did not meet the criteria for PTSD, had also experienced extremely stressful events in their lives.
During the study, Dr. Malan-Müller and fellow researchers found three distinct classes of bacteria that were unique in people with PTSD. Specifically, the names of the bacteria strains were Actinobacteria, Lentisphaerae, and Verrucomicrobia. The group of people with PTSD had lower levels of these strains.

Despite this finding, the study did not state a definite conclusion of “correlation” or “causation.” One possibility is that lower levels of these strains happen as a result of PTSD. Alternatively, having lower levels of these three strains may have predisposed these individuals to develop PTSD after experiencing a traumatic event.
Notably, individuals who had experienced trauma as children had lower levels of Actinobacteria and Verrucomicrobia. In addition to affecting brain health, these are also important bacteria for proper immune system function, which could help explain why children with traumatic experiences have more health problems.
The final hypothesis of Dr. Malan-Müller and her team is that “the low levels of those three bacteria may have resulted in immune dysregulation and heightened levels of inflammation in individuals with PTSD, which may have contributed to their disease symptoms.”
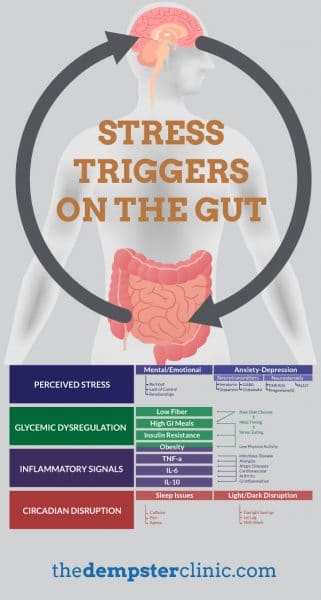
STRESS TRIGGERS ON THE GUT: PHYSICAL SYMPTOMS HAVE AN IMPACT, TOO!
An imbalanced gut has implications that extend beyond mental health. These additional symptoms can impede PTSD recovery, though. After all, it is already challenging for patients with PTSD to practice new coping skills and engage in sensitive talk therapy. Understandably, additional physical health problems may complicate a patient’s efforts even further.
In addition to disrupting mood regulation, an imbalanced gut microbiome also contributes to problems such as:
- Weakened immune system
- Skin disorders, such as eczema
- Digestive problems such as IBS, bloating, and constipation
- Chronic fatigue
- Impaired ability to fully absorb nutrients from healthy foods
- Difficulty sleeping
- Increased susceptibility to inflammatory diseases such as arthritis and heart disease
- Vulnerability to more allergies and food sensitivities
As you can see, healing the gut microbiome leads to a whole host of improved facets of wellbeing. There are many ways to naturally heal your gut. For example, eating fermented foods, drinking bone broth, regularly consuming prebiotics and probiotics, and reducing your sugar intake are all steps in the right decision.

HEAL YOUR GUT AND FEEL YOUR BEST AT THE HEALTHY GUT INSTITUTE
There are many steps you can implement right away to start healing your gut. However, especially for people with PTSD, the level of damage within their gut requires more specialized treatment and a more intensive learning program. An increasingly popular method of learning is through online courses, since they offer people the flexibility and comfort of treatment in their own homes.

I recommend considering the Healthy Gut Institute. This is a guided, step-by-step course with guided modules to help you be pain-free in six weeks or less. I created this course to help people achieve the well-balanced lifestyle they deserve. You may be tempted to hop around the internet reading various articles, hoping to find enough information to cobble together a plan to heal your gut. While this may seem like a good solution, the problem is that many of the articles you’ll find are out of date or written by unqualified individuals.
As a certified naturopathic doctor, I have created the most comprehensive gut program online. In fact, it is the only one that incorporates Functional Medicine, Integrative Medicine and Naturopathic Principles. The easy-to-implement training modules will result in high impact and life changing results. Please do not hesitate to visit the course page and scroll down to see video testimonials.
It may be especially helpful for individuals with PTSD to know that I offer exclusive mentoring through the course’s Private Healthy Gut Institute Facebook Group. This allows a safe space for you to ask questions without having to make a phone call or leave the house – which can understandably be very difficult in the early stages of PTSD recovery.
I encourage you to enroll today! Your best health awaits.
Dr. John Dempster, ND
The Dempster Clinic- Center for Functional Medicine

