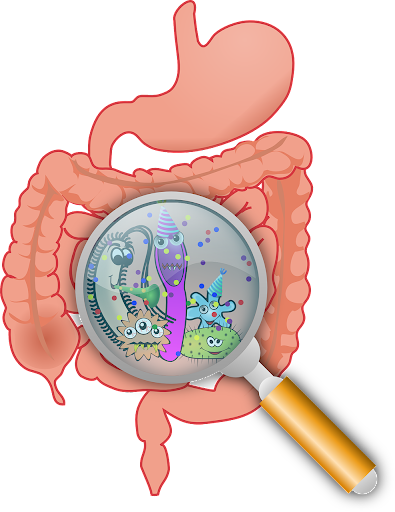
With over 100 trillion microorganisms in our gastrointestinal tract, gut microbiome health plays an undeniable role in our wellbeing. There is a vast diversity in the composition of the human gut microbiome which can differ based on age, sex, race/ethnicity, diet, etc. While these variations could be significant from person to person, it should be noted that there are core organisms that appear to exist across our GI tract.
Moreover, diversity of bacterial species has been suggested as an indicator of health. These include bacterial strains such as Bacteroides, Bifidobacterium, Lactobacillus, etc.
From metabolic function to gut-brain signaling, to regulation of anxiety, mood, cognition and inflammation these microorganisms participate in many of our body’s daily functions without us even realizing the role that they play. The only time we become aware of their existence is when something goes wrong.
Disbalance of gut microbiome can be caused by stress, illness, diet, antibiotics and aging and it is associated with physical and mental problems, including weight gain, depression, irritable bowel syndrome, inflammatory bowel disease, cardiovascular issues and various gastrointestinal disorders, including colorectal cancer.
The evidence supporting the role of the healthy gut microbiome in normal functioning of various pathways in our bodies is overwhelming. What’s more exciting is that this new knowledge about the linkage between gut microbes and health opens ways to new therapies and innovative ways of restoring gut health and thus improving our overall wellbeing.
One of such well-established methods for restoring gut health is fecal microbiota transplantation (FMT) or stool transplantation. FMT is a procedure which transfers fecal microbial samples from healthy human donors to the gastrointestinal tracts of patients with an array of gut related issues.
The stool transplantation methods vary and could include such procedures as duodenal infusion, colonoscopy, enema or frozen capsule transfer. While these procedures do not necessarily sound glamorous, it is the only microbe-based therapy that allows transfer of such a complex and diverse ecosystem into the GI tract.
While there are still questions about how FMT should be conducted, how effective it is long-term and whether the approach chosen for FMT should be disease specific – ongoing research in this area continues uncovering new knowledge which advances safe and efficient administration of FMT.
How does FMT work?
The idea of fecal microbial transplantation is fairly simple. The goal is to modify the existing composition of microbes in the gut, suppress certain unwanted strains, support others and overall, restore the balance of bacteria to a healthy level.
After demonstrating significant success in treating recurrent Clostridium difficile infection (rCDI), fecal microbiota transplantation has been tested for other diseases that stem from gut issues. Here is what scientific evidence has to say about effectiveness of FMT in treating different diseases:
FMT in Clostridium difficile infection (rCDI)
Recurrent CDI is an infection that people often develop when taking antibiotics or soon afterwards. It is called recurrent if it reemerges within eight weeks from the previous episode, which can be caused by the same or different type of bacteria. Recurrent CDI has been associated with high mortality with limited treatment options available. A 2020 metastudy analyzed a wide range of clinical data and research to determine the effectiveness of FMT in treating rCDI.
Extensive analysis of high quality evidence showed that FMT is effective for treating recurrent CDI, however delivery method and the number of administrations matter. Specifically, repeated FMT has an effectiveness of 91% after 8 weeks, while for single FMT effectiveness was 84%. From possible delivery methods, lower GI endoscopy was found to be the most effective (compared to delivery using enema or upper administration and other treatment options, such as vancomycin).
Overall, there is ample evidence proving the effectiveness of FMT in treating recurrent CDI. What about other gut issues?
2. FMT for irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD)
IBS and IBD are two diseases directly associated with changes in gut bacteria composition. This fact makes fecal microbiota transplantation a natural candidate for improving gut health and potentially treating these conditions.
In the case of IBD, there is particular promise when it comes to treating ulcerative colitis – which is a form of IBD. As for the IBS, randomized control trials show that there is some mixed evidence when it comes to alleviating symptoms like chronic abdominal pain and altered bowel habits. However, this can be attributed to the fact that there was high heterogeneity in terms of patient and donor characteristics, administration methods and number of infusions.
These results also suggest that the “right” donor might differ for different diseases. For example, patients that received stool enriched in specific strains of bacteria (like Lachnospiraceae and Ruminococcus) had better results. Also, high diversity in bacterial composition and presence of anti-inflammatory bacteria are additional factors that improve outcomes. However, different bacterial species might be preferred for IBS vs. IBD.
Overall, while there are mixed results about the effectiveness of FMT for IBD and IBS patients, these inconclusive results are caused by high variability in various factors. If patients’ individual characteristics are appropriately matched with those of donors and stool samples, FMT can be extremely successful. Thus, choosing appropriate doctors with sufficient knowledge and experience is paramount when opting for FMT.
3. FMT and Crohn’s disease
Crohn’s disease is a chronic inflammatory bowel disease characterized by inflammation of the digestive tract, which is believed to be a result of abnormal immune response to the gut microbiota. FMT aims to alter the composition of the gut bacteria to reduce the symptoms.
Studies about the effectiveness of FMT in Crohn’s disease have produced mixed results. There is definitely some evidence supporting the positive role of FMT in improving the symptoms, however some studies show no effect of the treatment.
Similar to IBS and IBM these mixed results can be explained by variability in factors like selection of donors, the preparation of fecal material, the delivery method, etc. The variability in study design and patient populations makes it difficult to draw definitive conclusions.
However, it should be noted that generally FMT is a very safe procedure, with the most common side effects being temporary GI symptoms, which makes it worth exploring FMT options and how successful it could be in your case, given your characteristics.
4. FMT and metabolic disorders
There is ongoing research exploring the use of FMT in metabolic disorders like obesity and metabolic syndrome. Some studies have suggested potential benefits, such as improved insulin sensitivity and weight loss, but further investigation is required.
5. FMT as a substitute for antibiotics
In addition to restoring gut microbiomes, FMT can be used as an alternative to antibiotics. FMT offers an alternative approach to treating certain bacterial infections, particularly those caused by multidrug-resistant organisms. Instead of relying solely on antibiotics, which can have side effects and contribute to antibiotic resistance, FMT aims to restore a healthy microbial balance and eliminate the need for long-term antibiotic use.
Where to start on your journey to a healthy gut?
As healthcare providers advance their understanding of benefits of fecal microbiota transplantation for an array of gut diseases, I would like to reiterate the importance of a healthy gut. There is so much you can do for your gastrointestinal health, starting from modifying your diet to comprehensive stool analysis, to fool allergy evaluation to SIBO testing. All of these components can illuminate the root cause of your disease and help you achieve optimal health.
If you are struggling with digestive issues such as IBS, IBD, SIBO, colitis, Crohn’s disease, Leaky Gut and others, I recommend considering the Healthy Gut Institute. This is a guided, step-by-step course with guided modules to help you improve your gut symptoms in six weeks or less. I created this course to help people achieve the well-balanced lifestyle they deserve.
As a licensed naturopathic doctor, I have created the most comprehensive gut program online which is completely based on Functional Medicine, Integrative Medicine and Naturopathic Principles. The easy-to-implement training modules will provide high impact tools to give you a chance for life changing results.