Many don’t know that autoimmune diseases (AD) are the third most common type of disease in the US after cancer and cardiovascular disease. The primary function of the immune system is to protect us from infectious agents, such as bacteria, viruses, toxins and cancer cells. This is accomplished with the help of antibodies – proteins that work against foreign bodies. An autoimmune disorder occurs when the body’s immune system can’t differentiate between your cells and potentially harmful foreign cells and starts attacking healthy body tissue. As a result, AD is among the most severe conditions that can turn your life upside down.
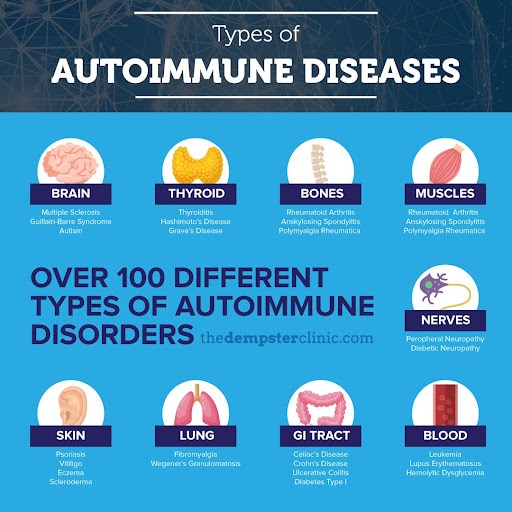
There are more than 100 types of autoimmune disorders with multiple sclerosis, Crohn’s disease, Type I diabetes, arthritis, thyroid diseases, inflammatory bowel disease (IBD) and Celiac disease being the most common ones.
The symptoms of these conditions can range from mild to extremely severe, with some of the common symptoms being fatigue, swollen glands, skin problems, joint pain, shortness of breath, digestive issues, etc. What makes AD so serious is that it can result in destruction of body tissue and abnormal organ growth and function.
What Causes an Autoimmune Disease?
Exact cause of autoimmune disease is still a mystery… but at least we know the risk factors that increase the probability of an autoimmune disease. These risk factors seem to stem from genetic predisposition combined with dietary, lifestyle and environmental factors – a perfect storm if you will.
The environmental risk factors are well researched and include gender, weight, smoking, medications and having one autoimmune disease. Let’s dive deeper into each of the risk factors:
- Gender: statistics show that 78% of people affected by autoimmune diseases are women. For certain types of autoimmune diseases, like lupus (SLE), this number can go as high as 95%. What can explain this huge disparity? Well, on the one hand, women tend to have a stronger antibody response, which protects them from infections. But, on the other hand, a higher number of antibodies increases the risk of developing autoimmune diseases, which possibly explains why ADs are more common among women.
- Weight: studies show that obesity is a major factor contributing to development of AD. Having higher BMI and more particularly fat, increases the body’s inflammatory response, which can contribute to the development of AD. Not only that, it can also cause more severe types of autoimmune diseases.
- Existing autoimmune disease: turns out having one type of autoimmune disease increases the risk of developing others. It is not uncommon for people to have 3 autoimmune diseases at once.
- Smoking: not surprisingly, smoking has been linked with autoimmune diseases like MS, lupus and others. Burning tobacco produces thousands of toxins, which trigger an immune response that can lead to development of an AD.
- Certain blood pressure medications and antibiotics have been shown to trigger development of autoimmune diseases.
Are Autoimmune Diseases Really on the Rise?
A study published in April, 2020 has shown that an increasing number of Americans have a high prevalence of antinuclear antibodies (ANA) in their blood. While there are a number of biomarkers for AD, ANA is the most commonly used to signal the risk of developing autoimmune disease. The increase was especially pronounced in three groups: non-Hispanic white males, adults over 50 and adolescents.
“Growing evidence suggests that the ANA precede the onset of autoimmune disease; thus, ANA may be a marker or may signal increased susceptibility to autoimmune diseases,” the researchers explained.
Considering that human genetics hasn’t changed much in the past 30 years, it is likely that the increase in antibodies (and thus in autoimmune diseases) is triggered by changes in environmental factors and/or lifestyle. One of the possible explanations is increased consumption of processed, high fat and high sugar foods, which are known triggers of inflammation and immune response..
Another factor contributing to the rise of autoimmune disease is an imbalance, or disturbance, of our gut microbiome. Studies are actively discussing the link between gut health and immunity. Disturbance of gut microbes, which is often caused by antibiotics (via prescription or food route), can change our microbial composition, weaken our immunity and provoke several autoimmune diseases. According to “hygiene hypothesis” children are not exposed to germs as much any more, which causes their immune system to overreact in case of even harmless triggers.
What Can We Do?
It should be noted that we still have control over the health of our immune system. By paying attention to your diet and strategically including foods rich in certain nutrients, you will give your immune system the fuel it needs to stay strong and healthy. There are six specific nutrients that can help reduce your risk of autoimmune disease. These include magnesium, Omega-3 Fatty Acids, Vitamin D and others. As I regularly mention, it is best to uncover your unique deficiencies via testing to help sculpt a program unique to you. There are also various medications for AD that alleviate the symptoms.

Maintaining a healthy gut and incorporating the aforementioned nutrients into your diet is key for preventing autoimmune disease and protecting your overall health. However, designing a sustainable meal plan that fits your specific needs, promotes healthy intestines, and checks off all the right boxes can be incredibly challenging. At The Dempster Clinic – Center for Functional Medicine, I will work with you to create the best nutrition plan for you based on your own unique health concerns.
We also offer comprehensive autoimmune screening, which is an economical and efficient way to assess possible tissue damage to multiple organs of the body. It measures for predictive antibodies, some of which can appear up to ten years before the clinical onset of disease. Predictive antibodies help with identification of markers and possible precursors of autoimmune diseases.
This screening provides a detailed assessment that includes a wide range of different antigens. It is recommended for patients who have a diagnosed autoimmune disorder, as they commonly develop additional autoimmune conditions. As well as, for those who have chronic increased intestinal permeability, which is the gateway for environmentally induced autoimmune disorders.

